We all know what ICD-10 is; its more than updated codes, it is how a provider can now define care more descriptively. It has laterality, now 7 digits, captures specificity, extensive parameters and even uses combination codes to better capture complexity of the diagnosis.
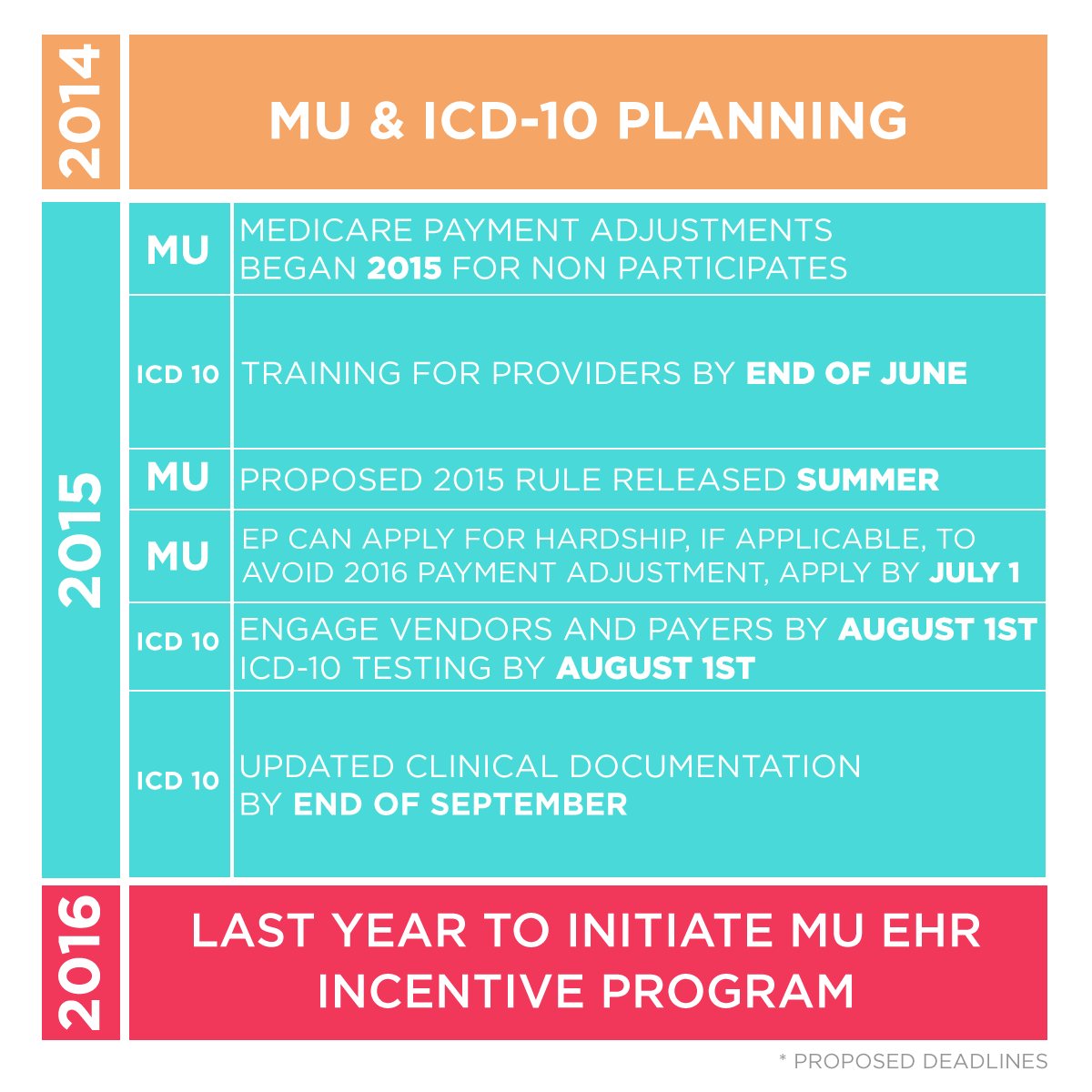
With ongoing Meaningful Use changes and ICD-10 right around the corner where is your organization in this timeline?
Our MU and ICD-10 Experts can now assist you with achieving any of these items. We offer consultants that can lead these processes for you or just fill in the gaps where you need it. We offer a PRN/As Needed program that allows you to use the hours when you need them. 5, 10, 20 hours, whatever you need.
Contact us today!
1-888-674-0999 or email us at info@ehrconcepts.com.
So what should your organization be doing to prepare?
- Pinpoint the ICD-9 codes you use most frequently
- Reviewing superbills, encounter forms, practice management reports, and the Common Codes then create an action plan.
- Provide Coding Education
- Documentation training for providers and staff who document in the patient medical record
- Coding training for staff members who work with codes on a daily basis
- Improve Clinical Documentation, Paper Forms and Templates
- Optimize, design and edit your note templates to include the appropriate information needed to support the ICD-10 selected
- Test Your Systems and Processes
- Create Test scenarios
- Find 10 existing encounters/claims to test
- Identify ICD-10 codes for each scenario and use difference dates of service
- Conduct External Testing with Partners
- Verify submittals, received and process of data that contains ICD-10 codes
- Practice and Validate through CMS testing
- Last testing week in July